
Medically Underserved Areas and Populations
Overview
Medically Underserved Areas/Populations and GME
Consistent with its mission to improve health care and population health, the ACGME seeks to enhance physician workforce development in communities that face physician shortages in various specialties.
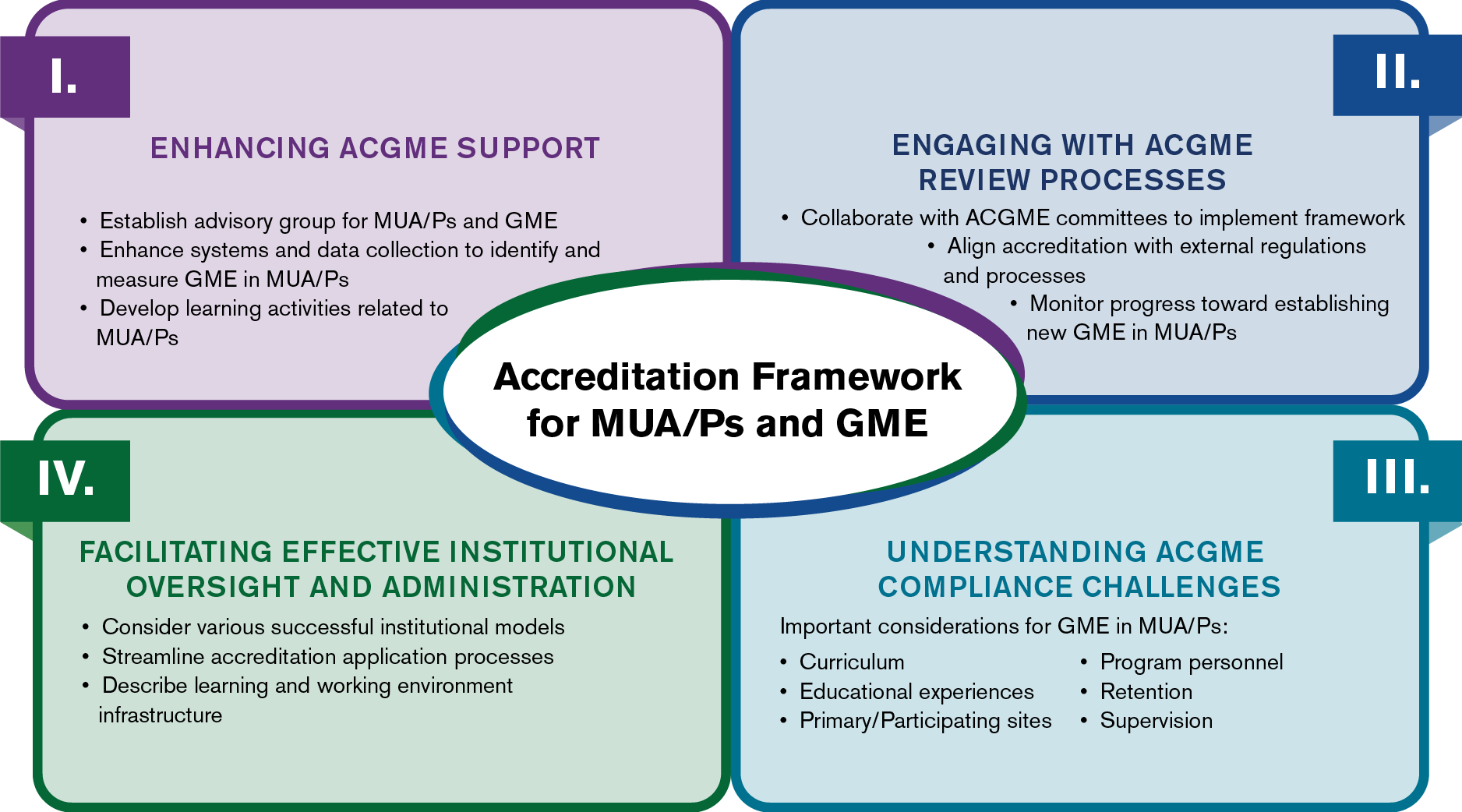
As part of this effort, the ACGME developed a framework to encourage the development of graduate medical education (GME) that will result in enhanced access to and availability of health care in medically underserved areas (MUAs) and medically underserved populations (MUPs). Medically underserved areas and populations (MUA/Ps) are places or communities in which groups of people have unmet health or health care needs.
This framework outlines initial actions addressing graduate medical education in MUA/Ps.
Concurrent Application Pilot
In alignment with the ACGME’s framework for MUA/P and GME, the ACGME is establishing a pilot program aimed at expediting the review of Sponsoring Institution and program applications, particularly for those with a mission to serve MUA/Ps. This process would allow a Sponsoring Institution and program to submit applications at the same time in the Accreditation Data System (ADS), and to receive both institutional and program accreditation decisions within a nine-12-month period.
The pilot period will last for one year, from July 1, 2025 to June 30, 2026, and will accept up to 12 new Sponsoring Institutions.
Learn more and read FAQs.
MUA/P Advisory Group
The ACGME has an advisory group to advise the ACGME on implementation of the framework for medically underserved areas/populations (MUA/P) and graduate medical education (GME). Learn more.
Rural Initiatives
ACGME Rural Track Program Designation
Consistent with Section II of the MUA/P framework, the ACGME has developed processes addressing ACGME-accredited programs that seek to create “rural tracks” as defined in rules and regulations of the Centers for Medicare and Medicaid Services (CMS) in 42 CFR §413.79(k), including an ACGME Rural Track Program designation that is available both for an existing program (with a permanent complement increase and new rural site(s)) or as part of the application for a new program. Visit the Rural Track Program Designation web page to learn more.
Rural Health Matters
ACGME Past President and CEO Thomas J. Nasca, MD, MACP joined University of Nebraska Medical Center and University of Nebraska Omaha Chancellor Jeffrey P. Gold, MD on RFD-TV’s Rural Health Matters in April 2021 to discuss the COVID-19 pandemic’s effects on rural America, GME, physician well-being, the current state of the US health care system, and more. In this excerpt, Dr. Nasca describes pathways for new physicians who want to serve rural communities and the role of academic partnerships in providing education to address health care needs.
Evaluating Teaching Health Center Planning and Development: Unlocking and Sustaining the Full Potential of the Teaching Health Center Program
E.M. Hawes et al., June 2025
Virtual Interviews: Concerns for Rural Residency Programs
D. Waldman et al., June 2025
Training More Physicians for Medically Underserved Communities: The Power of Regional Medical Education Collaboratives Across the Training Continuum
M.L. Tran-Reina et al., May 2025
Recruitment of Residents to Rural Programs: Early Outcomes From Cohort 1 of the Rural Residency Planning and Development Grants Program
A. Weidner et al., August 2024
Housing Challenges and Opportunities for Rural Residency Development
A.J. Zolotor et al., August 2024
The Teaching Health center Graduate Medical Education Program: A Permanent Funding Imperative
A.P. Philips et al., August 2023
Establishment of a Fellowship in Street Medicine
M. Kiazand et al., June 2023
The ACGME Framework for Medically Underserved Areas and Populations and Graduate Medical Education
L. McDougal et al., April 2023
Graduate Medical Education Training and the Health of Indigenous Peoples
M.J. Owen et al., February 2023
A Scoping Review of Indigenous Health Curricular Content in Graduate Medical Education
M. Rashid et al., February 2023
Avoiding Unethical Altruism in Global Health: Revisiting Ethics Guidelines for International Rotations for Medical Residents
S.R. Ross et al., February 2023
Vulnerable yet Unprotected: The Hidden Curriculum of the Care of the Incarcerated Patient
M.I. Suh et al., December 2022
Evaluating the Teaching Health Center Graduate Medical Education Model at 10 Years: Practice-Based Outcomes and Opportunities
C. Smith Davis et al., October 2022
It’s Time to Stop Pointing Fingers: The Role of GME in Addressing the Issue of Unmatched US Medical School Graduates
K.M. Andolsek et al., August 2022
Family Medicine Residencies: How Rural Training Exposure in GME Is Associated With Subsequent Rural Practice
D.J. Russell et al., August 2022
CMS Finalizes Rules for Distribution of 1000 New Medicare-Funded Residency Positions and Changes to Rural Training Track Programs
K. Schleiter Hitchell et al., April 2022
Federal Bills Raise Cap on Medicare-Funded Residency Positions and Modify Graduate Medical Education Policies
K. Schleiter et al., August 2021
Rural Residency Training as a Strategy to Address Rural Health Disparities: Barriers to Expansion and Possible Solutions
E.M. Hawes et al., August 2021
Cultivating Healthy Governance in Rural Programs
R. Longenecker et al., April 2021
Rural Workforce Years: Quantifying the Rural Workforce Contribution of Family Medicine Residency Graduates
P. Meyers et al., December 2020
A Roadmap to Rural Residency Program Development
E.M. Hawes et al., August 2020
Developing Graduate Medical Education Partnerships in American Indian/Alaska Native Communities
M.A. Sundberg et al., December 2019
Community Health Center Engagement and Training During Obstetrics and Gynecology Residency
A.Y. Cheng et al., October 2019
Preparing Physicians for Rural Practice: Availability of Rural Training in Rural-Centric Residency Programs
D.G. Patterson et al., October 2019
International Medical Graduates in the US Physician Workforce and Graduate Medical Education: Current and Historical Trends
A.A. Ahmed et al., April 2018
A Free Clinic Continuity Experience During Residency Is Associated With Practice in Underserved Areas
S.M. Petrany et al., October 2017
Teaching Health Center Graduate Medical Education Locations Predominantly Located in Federally Designated Underserved Areas
S.C. Barclift et al., May 2016
Boston Health Care for the Homeless Program – Harvard Dermatology Collaboration: A Service- Learning Model Providing Care for an Underserved Population
J. Sheu et al., December 2014
Impact of Global Health Experiences During Residency on Graduate Practice Location: A Multisite Cohort Study
W. Liaw et al., September 2014
Rural Primary Care Physician Workforce Expansion: An Opportunity for Bipartisan Legislation
R.E. Rieselbach et al., December 2013
A Pilot Curriculum to Integrate Community Health Into Internal Medicine Residency Training
J. Catalanotti et al., December 2013
Resident Education in Free Clinics: An Internal Medicine Continuity Clinic Experience
A.T. Pincavage et al., June 2013
An Experiential Community Orientation to Improve Knowledge and Assess Resident Attitudes Toward Poor Patients
E.A. Wallace et al., March 2013
County Jail as a Novel Site for Obstetrics and Gynecology Resident Education
C.B. Sufrin et al., September 2012
Residents’ Attitudes and Behaviors Regarding Care for Underserved Patients: A Multi-Institutional Survey
M.L. Wieland et al., September 2011
An International Health Track Is Associated With Care for Underserved US Populations in Subsequent Clinical Practice
A.W. Bazemore et al., June 2011
Reflective Practice and Competencies in Global Health Training: Lesson for Serving Diverse Patient Populations
J. Castillo et al., September 2010
