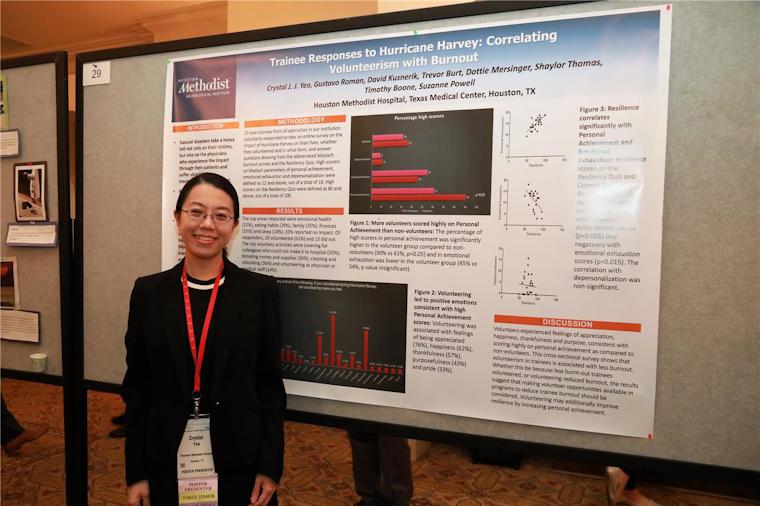
Crystal Jing Jing Yeo, MD, PhD, MRCP(UK), a neurology resident in her final year of residency, came to the Annual Educational Conference as a poster presenter. Her poster on Trainee Responses to Hurricane Harvey: Correlating Volunteerism with Burnout was selected from among numerous responses to the ACGME’s Call for Abstracts for presentation at the 2018 Annual Educational Conference. We spoke with Dr. Yeo about her project and future plans at the Poster Reception on Thursday evening, March 1.
ACGME: Tell us about your academic and professional role.
Dr. Yeo: I'm a final year neurology resident at the Houston Methodist Hospital, Texas Medical Center.
My other roles are serving as a young physician leader on hospital GME committees, as well as regional and national committees in the United States, including those of the AANEM, Texas Medical Association (TMA) and TEXPAC, and acting as a Harris County Medical Society Alternate Delegate to the TMA House of Delegates.
ACGME: Can you briefly describe your project for us?
Dr. Yeo: Professor Suzanne Powell and I wished to explore the impact of Hurricane Harvey on entering trainees, including transfer residents and fellows, and whether resilience and burnout was different in those who volunteered help during the natural disaster. The natural disaster was a unique and immense high-stress situation, which, on top of the first-year struggles, put the entering trainees at high risk of vicarious traumatization and burnout.
Vicarious traumatization refers to emotional distress caused by empathy. We expected physicians to volunteer to help out of compassion, the hallmark of our profession, a hallmark which sadly is lost as a consequence of burnout. Volunteering is associated with physical and mental well-being, and we hypothesized that volunteering would be associated with decreased burnout in trainees.
We used a cross-sectional survey to measure association between volunteering, resilience, emotional exhaustion (which means emotional and physical fatigue), depersonalization (which means cynicism), personal achievement (which means feelings of adequacy). The results were gathered through a self-administered online questionnaire via Survey Monkey.
ACGME: What inspired you to do this project?
Dr. Yeo: In my specialty of neurology, I see patients with terminal illnesses, such as dementia and ALS, which leave them very debilitated. These illnesses take a great toll not only on the patients, their families, and caretakers, but also on physicians who are dedicated to their care. I wish to provide supportive measures for all these individuals. I am concerned about how burnout affects the ability of physicians to care for patients, especially those whose families are in need of compassionate support as well.
As a trainee myself, I think that it is important to intervene at an early stage. At the individual level, helping young physicians gain important life skills, which increase resilience and decrease burnout, will set them up for the rest of their career. Such life skills might include time-management skills, stress-coping skills, and mindfulness, which means attending to and consciously reacting to the present moment. Trainees are often too junior to be in a position of power to change stress-inducing organizational or government policies; however, they can use stress-coping skills. These skills are directly relevant to our profession, which has been always a stressful one even before “physician burnout” became a buzzword. When trainees gain seniority, the same skills will enable them to be change-makers.
At the professional level, it addresses attrition from the workforce from an early stage. Once the profession has a critical mass of physicians with high resilience, these physicians can coach and develop younger colleagues, thereby changing the culture.
ACGME: What did you discover?
Dr. Yeo: We found that the group who volunteered during Hurricane Harvey had significantly fewer trainees who scored lowly in personal achievement, which, together with emotional exhaustion and depersonalization, is a marker of burnout. Volunteering was associated with feelings of being appreciated, happiness and purpose.
When comparing the three burnout measures with resilience, we found that personal achievement strongly correlated with resilience, while emotional exhaustion negatively correlated with resilience, and depersonalization was not associated with resilience. Psychological distress strongly correlated with emotional exhaustion, and negatively correlated with resilience.
It was surprising that only personal achievement was significantly different between volunteers and non-volunteers. Although emotional exhaustion is thought to correlate best with burnout, the reality is that burnout is a multi-dimensional syndrome involving all three measures. Feelings of personal achievement and competence have been shown to be directly linked to job satisfaction, fewer medical errors and better patient care. Since personal achievement can be increased by supportive measures, such as constructive feedback and good social support, it is an important issue to address.
ACGME: What was the main takeaway what is next?
Dr. Yeo: The once-in-a-lifetime impact of Hurricane Harvey on new trainees was explored in this cross-sectional survey, which showed a significant association between volunteerism and a greater sense of personal achievement. Personal achievement was strongly associated with resilience, which in turn was protective against psychological distress. There is potential for this cross-sectional survey to be extended to other trainees who have already been working in the institution, attending physicians, and other medical staff. Since a cross-sectional survey cannot establish causality, scientific rigor would demand that a randomized controlled trial be conducted to see if a regular volunteer program and a volunteer program during disaster management reduces or prevents burnout.
ACGME: Who could benefit from this?
Dr. Yeo: This study suggests that structured volunteer opportunities during critical disaster management and beyond should be explored and offered not just in graduate medical education programs targeting resident burnout, but also in wellness programs for attending physicians and other medical staff, as well as including volunteer work in disaster management plans. Volunteering is an excellent way to help the community and the physicians at the same time.
ACGME: Any additional follow-up plans?
Dr. Yeo: Future directions would include enrolling a bigger sample size to provide more statistical power, by including trainees at all levels, physicians, and other medical staff. Given that this is already the fourth such natural disaster impacting Houston in almost 20 years, with Tropical Storm Allison in 2001, Hurricanes Katrina and Rita in 2005, and Hurricane Irma in 2008, it would be highly relevant for the study cohort to be extended to all physicians and trainees in the Texas Medical Center, to enable all institutions in the area to collaborate on lessons learned and optimize critical disaster management plans. Our findings suggest that there are benefits of including volunteer work in disaster management plans. A prospective randomized control trial would be instrumental in evaluating the relationship between volunteering, personal achievement, resilience and psychological distress. Our institution is spearheading a multi-disciplinary task force to look into multi-center research and measures to target systems deficits and improve physician resilience and wellness.