Recognizing the high rates of psychological distress of various forms for residents in training, Dr. Gregory Guldner and colleagues sought to learn whether an opt out approach would increase the number of residents who actually engaged with available therapy options. They presented their work in the Poster Hall at the 2022 ACGME Annual Educational Conference, which was held virtually March 30-April 1, 2022.
Poster: Opt-Out Versus Opt-In Therapy Sessions for Residents Increases Resident Use of Ongoing Therapy by 400%
Authors: Gregory Guldner, MD, MS; Timothy Sisemore, PhD; Deborah Streletz, MD; Alina Popa, MD; Napatkamon Ayutyanont, PhD; Joshua Fuller, PhD; Chandler Broadbent, MA; Jason Siegel, PhD
ACGME: Can you tell us about your academic and professional role?
Dr. Guldner: I currently serve as the DIO at HCA Healthcare Riverside in southern California and the Lead Physician for HCA GME National Wellness Committee. I am also a clinical professor of emergency medicine at the University of California Riverside School of Medicine.
ACGME: Can you briefly describe your project for us?
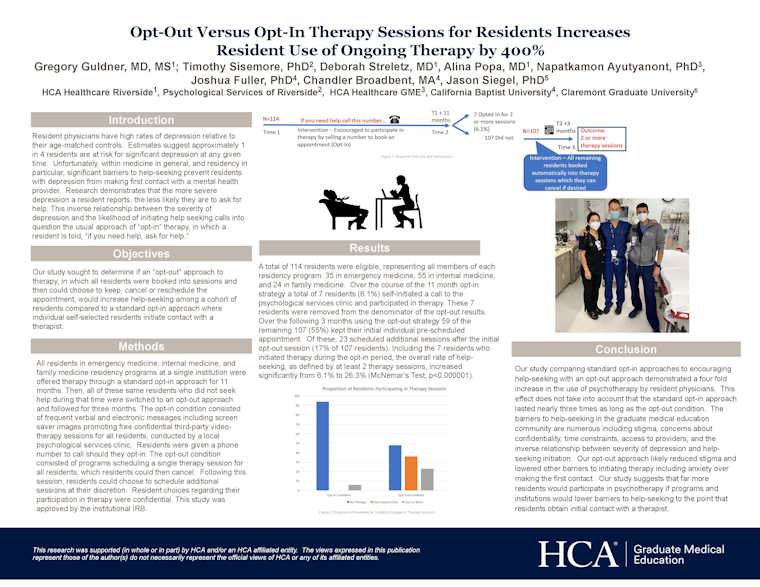
Guldner: We compared the usual "opt-in" approach to therapy, where residents are told who to call should they need help, to an "opt-out" approach where residents were scheduled into a therapy session that they could then cancel if they felt it unnecessary. We compared the use of therapy during 11 months of standard "opt-in" among all residents in family medicine, internal medicine, and emergency medicine to the use of therapy after initiation of the opt-out program. The clinic providing tele-therapy services reported only aggregated data to the researchers during both phases. We defined ongoing therapy during the opt-out phase as any resident who opted to continue therapy at the end of the initially scheduled session.
ACGME: What inspired you to do this project?
Guldner: The literature describes high rates of psychological distress of various forms for residents in training, yet the stigma associated with actually asking for help, as required by the "opt-in" approach, often prevents residents from initiating contact with a therapist. Furthermore, research shows that the more depressed residents are, the less likely (not more likely) they are to seek help. This paradox almost ensures the failure of opt-in approaches. Much like the military and law enforcement we sought to determine if opt-out approaches would be more effective.
ACGME: What did you discover?
Guldner: We had 114 eligible residents. Over the 11 months of the standard opt-in approach, six percent initiated therapy. In the three months during which we initiated the opt-out approach, we found that 55 percent of all residents kept their initial scheduled appointment and 26 percent of residents continued therapy beyond the initial session.
ACGME: What was the main takeaway?
Guldner: Asking residents to "call if you need help" does not work well in the GME environment. Opt-out approaches significantly increase the use of therapy, likely by both lowering stigma and facilitating the initial contact with a therapist.
ACGME: Who could benefit from this?
Guldner: We believe all residents and fellows could benefit from a program that helps lower stigma associated with help seeking.
ACGME: Any additional follow-up plans?
Guldner: We are looking at the rate of therapy use a year following the three-month opt-out implementation. We believe that having had even a single session likely lowered barriers to later therapy even if residents did not choose to continue at that time. We hope to expand this approach to other institutions and residency programs.