Oklahoma has a primary physician shortage, particularly in rural and tribal areas. Natasha Bray, DO, MSEd and colleagues explored how completing a residency in these underserved areas affects independent practice location choice in a continuation and expansion of a previous study. They presented their work in the Poster Hall at the 2022 ACGME Annual Educational Conference, which was held virtually March 30-April 1, 2022.
Poster: Addressing Physician Shortage in Medically Underserved Rural and Tribal Communities Through Residency Program Collaboration
Primary Author: Natasha Bray, DO, MSEd
Co-Authors: Douglas Nolan, DO; Ashton Clayborn, DO; Daniel Molina, MD
ACGME: Tell us about your academic and professional role.
Dr. Bray: I am the interim dean of Oklahoma State University (OSU) College of Osteopathic Medicine – Cherokee Nation Campus and the associate dean for accreditation for OSU Center for Health Sciences. I am board certified in internal medicine and addiction medicine. I have previously served as an internal medicine program director and DIO [designated institutional official]. I am the current Chair of the ACGME’s Council of Review Committee Chairs and serve on the National Residency Match Program (NRMP) Board of Governors.
ACGME: Can you briefly describe your project for us?
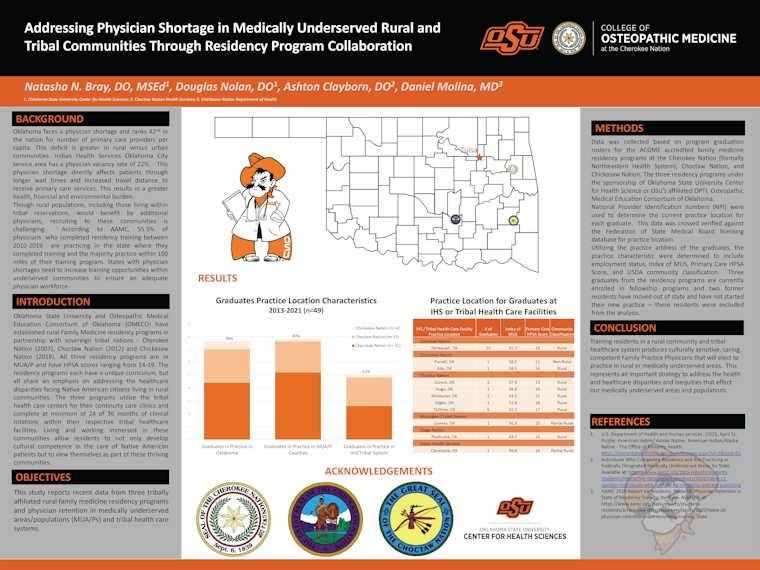
Bray: The project reviewed graduates from three tribal/rural family medicine residency programs to determine if completing a residency in a rural location would encourage graduates to practice in medically underserved/tribal communities. Oklahoma has a severe primary care physician shortage, and this shortage disproportionately affects our rural communities and Native American Tribal Health Care Centers. OSU Center for Health Sciences has been establishing residency programs in rural communities and in association with indigenous tribes in Oklahoma since 2007. We wanted to examine the practice patterns of the graduates of these programs to determine if the remained in rural and underserved communities for practice.
ACGME: What inspired you to do this project?
Bray: We started the project to determine if establishing rural residency programs would be a viable solution to the physician shortage that affects health care in rural Oklahoma communities.
ACGME: What did you discover?
Bray: Eighty percent graduates practice in medically underserved areas/populations (MUA/P). As of June 2021, 49 family medicine physicians have graduated from these programs. Thirty-nine (80%) are practicing in MUA/P counties and 25 (51%) are in practice with Indian Health Services or a Native American Tribal Health Care system.
ACGME: What was the main takeaway?
Bray: Establishing primary care residency programs in rural/underserved locations is beneficial to improving health care disparities for MUA/P. The value of the longitudinal nature of the study is the ability to demonstrate that graduates are remaining in these communities up to nine years after completing residency. Given the difficulty to recruit and retain physicians in rural and underserved communities, increasing education opportunities in these environments represents an important strategy to address physician shortages and maldistribution.
ACGME: Who could benefit from this?
Bray: Rural areas, Native American/Indian health service facilities, Veterans Affairs—any medically underserved areas that have difficulty with recruiting and retention of a physician workforce.
ACGME: Any additional follow-up plans?
Bray: OSU has developed a rural track for the pediatric residency program with the first class of residents to graduate in 2025. We intend to follow the current programs involved in this project with the addition of the pediatric rural track graduates to determine if the results are similar.