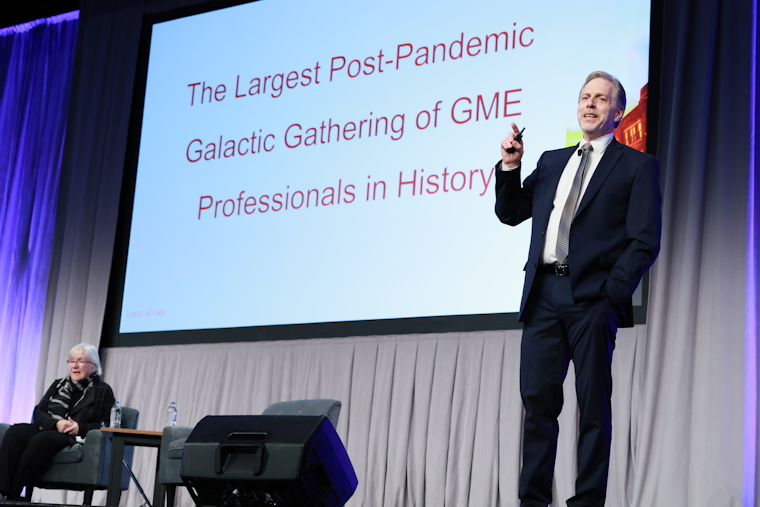
ACGME Chief of Staff and Chief Education Officer Timothy P. Brigham, MDiv, MS, PhD welcomed attendees to the ACGME’s first in-person conference in 1,091 days to kick off the second day of the 2023 Annual Educational Conference. The energy in the room picked up on the celebratory atmosphere of the previous evening, reflecting how excited members of the graduate medical education (GME) community are to be together connecting, learning, and inspiring each other. ACGME Board of Directors Chair Claudia Wyatt-Johnson, the first Public Director of the Board to serve in the role, rounded out the Welcome Address by presenting the John C. Gienapp Award to Elias Traboulsi, MD of the Cleveland Clinic and then introducing ACGME President and CEO Thomas J. Nasca, MD, MACP for his President’s Plenary.
Dr. Nasca’s comments were organized into three areas: the aggregate numerical relationship between undergraduate and graduate medical education (addressing the question of whether there are enough pipeline positions for the number of medical school graduates); an update on his categorization of three simultaneous pandemics and the role of health care in addressing those; and a discussion of the path forward for GME as he sees it.
“If we fail to do… if we fail to address… things will not get better,” he said. He challenged the audience not to “expect others to make the change,” noting “we can make a difference and be the change.”
Following the President’s Plenary, attendees chose from four Featured Plenaries.
Roe v. Wade and the Future of Graduate Medical Education
The 2022 US Supreme Court decision in Dobbs v. Jackson Women’s Health Organization rendered some of the requirements in the ACGME Program Requirements for Graduate Medical Education in Obstetrics and Gynecology illegal in states overnight, a first for the ACGME, said ACGME Senior Vice President, Accreditation Mary Klingensmith, MD, who moderated this featured plenary. After the decision, the Review Committee for Obstetrics and Gynecology, along with ACGME leaders, determined that ACGME-accredited programs must still teach residents abortion care no matter the program location.
“Our duty is to train our graduating residents to be able to practice anywhere,” said panelist Gabriella Gosman, MD, who chairs the Review Committee, explaining the rationale for reinforcing the importance of the existing requirements.
Gynecologic oncologist Dineo Khabele, MD said her program at Washington University in St. Louis had to work with institutions in Illinois so residents could rotate there, but also had to educate non-obstetrician-gynecologist colleagues locally and assure them they can care for pregnant patients without criminal ramifications.
“There is a lot of fear and it’s understandable,” Dr. Khabele said,” but we don’t want there to be a spillover effect where this affects other aspects of health care.”
The NAM Plan for Health Workforce Well-Being: An Interview with the US Surgeon General
“Generosity, service, love—those are the values we should have.” These words drove home the overarching message of this powerful plenary, in which Dr. Brigham; National Academy of Medicine (NAM) President Victor Dzau, MD; and US Surgeon General Vivek Murthy, MD, MBA discussed the collaborative efforts of medical education organizations in the continued effort to enhance physician well-being. In a video presentation, Dr. Dzau provided background on the NAM National Plan for Health Workforce Well-Being. This was followed by a virtual interview between Drs. Murthy and Brigham.
They discussed that burnout is a crisis that pre-dated the COVID-19 pandemic. The pandemic, however, intensified demands and lengthened clinicians’ work hours, creating new challenges. The NAM National Plan is attempting to create a movement to combat this reality. Powerful applause followed the statement of a core principle: that the lives and well-being of clinicians matter too.
Preparing Learners to Care for Patients and Communities Experiencing Substance Use Disorder
Panelists in this plenary gave impassioned presentations on caring for patients with substance use disorders (SUDs). Calling it one of the most pressing matters of our time, Jeanette Tetrault, MD, FACP, FASEM lamented that only one out of 10 people experiencing SUD will receive care.
Charlene Dewey, MD, MEd, MACP stressed the importance of avoiding terminology that may perpetuate stigma, especially by clinicians and institutions, a message emphasized throughout the session. Stigmatizing language may shame or guilt SUD patients, driving them away from seeking care. Dr. Tetrault underscored this message, calling stigma “pervasive and damaging.”
In an emotional presentation, Stephen Loyd, MD compared his own SUD challenge to that of one of his patients, humanizing and personalizing the experience and challenge faced by those experiencing SUDs in dealing with systemic barriers to care. Few eyes remained dry by the time his presentation concluded, when he argued that the care he received “should be the norm [and should] not be the exception."
Nutrition and Health: Developing a GME Framework
The more nutrition education is shared with physicians, the more counseling they do with patients, a panel of nutrition experts emphasized in this plenary. While physicians may be familiar with general nutrition statistics and fundamentals, many are not receiving adequate education to feel confident to counsel patients, despite research showing that patients who receive even a small amount of advice see improved overall health outcomes.
ACGME Chief Communications and Public Policy Officer John Combes, MD introduced the session, noting the ACGME’s commitment to convening experts to address the medical education responsibility of nutrition health. He added that the ACGME will host a Nutrition Summit in March 2023 to further the discussion.
Panelists Kate Sommerfield, MPA; David Seres, MD, ScM, PNS, FASPEN; and Jaclyn Lewis Albin, MD, FACP, FAAP shared relevant statistics on health outcomes and food insecurity, stories of intervention, and historical context for nutritional guidelines; and gave helpful advice for those working with learners and patients.
“Knowing where our patients come from is how we help them,” said Dr. Albin, echoing sentiments from the other panelists about the importance of asking patients about food security and encouraging physicians to embrace their role as a reliable source for accurate nutritional information. “Who are the people to turn to if not a qualified health care professional?” asked Dr. Seres. “People follow guidelines to live longer, live healthier, and live happier. The stakes could not be higher. We must teach physicians.”
Meaning in Medicine: Making a Difference
The conference theme underpinned the educational sessions throughout the rest of the day. Topics included ACGME accreditation and initiatives; diversity, equity, and inclusion; professional development; well-being; crisis management; and other impactful subjects. Attendees networked during breaks, saw exhibitor demos and met with vendors as well as ACGME and ACGME International staff members in the Exhibit Hall, and continued sharing insights and experiences with each other. Activities and wellness opportunities helped balance out packed schedules. Saturday, the third and final day of #ACGME2023, promises more occasion for learning, sharing, and connecting, as well as two additional powerful presentations in the Marvin R. Dunn Keynote Address and the Closing Plenary.