This is one in a series of project profiles of the ACGME’s Back to Bedside initiative, which empowers residents and fellows to develop innovations that foster meaning and joy in work and engage their patients on a deeper level.
Surgical Rehearsal Platform (SRP) technology (also called “surgical theater”) is like taking a virtual reality tour through a complicated surgical procedure. It has become an essential teaching tool in many surgical graduate medical education (GME) programs across the country. The technology also helps surgeons practice the procedure before heading into the surgical suite.
The Back to Bedside team at Case Western Reserve University/University Hospitals Cleveland Medical Center, led by James Wright, MD and Christina Wright, MD, has found an additional use for this virtual reality technology: to make the informed consent process more meaningful to patients and to provide an opportunity for greater resident-patient interaction.
The vast majority of patients undergoing a surgical procedure sign an informed consent document that states they understand the risks and benefits of surgery. But most patients have little understanding of what actually is being done.
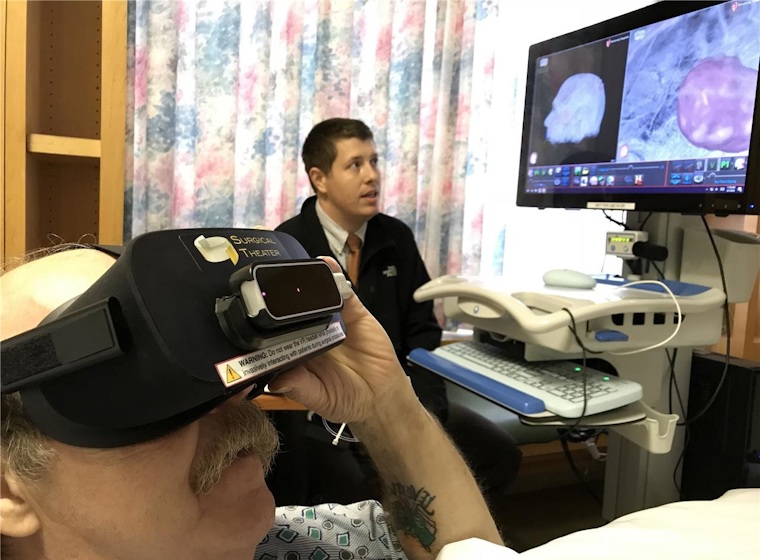
In this new consent process, the resident pre-loads the patient’s scans into the surgical rehearsal platform to create an interactive, three-dimensional view of that patient’s condition and surgery. With the touchscreen monitor at the bedside, the residents explain the plan for surgery while the patients wear a virtual reality headset to actually “look” at their own structures and follow what will happen during procedure.
The Back to Bedside team is collecting data from patients and residents, both with and without the SRP-aided informed consent. Across the board, the data shows statistically significant improvements in patient understanding of the procedure and trust in the surgeon. The responses show a clear correlation between the technology and patient satisfaction and comfort with their pending procedures.
“Not every patient wants this level of detail, and this is understandable because it can create some anxiety,” said project lead Dr. James Wright. “But those patients that do participate feel better. Also, their family members become more engaged and ask good questions.”
Dr. Wright said that one of the best aspects of this process is that it provides more one-on-one time with patients. “That’s been the most rewarding aspect of this--the quality time with patients.”
This project is part of the ACGME’s Back to Bedside initiative, which empowers residents and fellows to develop transformative ideas and projects that foster meaning and joy in work through deeper engagement with patients. The initiative provides financial and administrative support to innovations that can be broadly disseminated and solutions that can be implemented at multiple institutions. More than 60 projects across two cycles have received initial funding through Back to Bedside.
Back to Bedside was developed in response to the trend of patient care and academic learning occurring away from the patient bedside. External pressures, including administrative burdens, electronic health record requirements, production pressures, built-in inefficiencies, and other local influences are responsible for this shift in the delivery of medical education and patient care.
Back to Bedside hopes to support processes, initiatives, curricula, projects, and other activities designed and implemented by and for residents and fellows. By fostering activities that build a sense of meaning in work and reminding them of the reason they entered the profession in the first place, this initiative hopes to encourage all residents and fellows to look at how they can improve their learning environments.