This is one in a series of project profiles of the ACGME’s Back to Bedside initiative, which empowers residents and fellows to develop innovations that foster meaning and joy in work and engage their patients on a deeper level.
Greetings are important.
The power of using someone’s name when communicating has long been established as an important, if subconscious, element of building stronger one-on-one connections.
Calling patients or caregivers by their name is a simple but extraordinarily powerful gesture. It’s also the idea behind the Back to Bedside project at Children’s Hospital of Philadelphia (CHOP).
“Research showed that at CHOP, only about a third of the time residents, attending physicians, and nurses were calling caregivers by their names,” said Nathaniel Bayer, MD, who co-led the project with Jacobo Santolaya, MD and Sara Rosenbaum, MD. “We wanted to change that.”
The team believed that encouraging residents to use each parent’s or caregiver’s preferred name would bring some personal and human qualities back to the pediatric provider-parent relationship. And at the same time, resident burnout could be reduced by encouraging caregivers to call residents by their names as well.
Using a 16-bed general pediatric unit for the pilot, the team initially encouraged residents to call their patients’ caregivers by their names. But after a survey, the team found that more than half the caregivers would rather be called mom or dad.
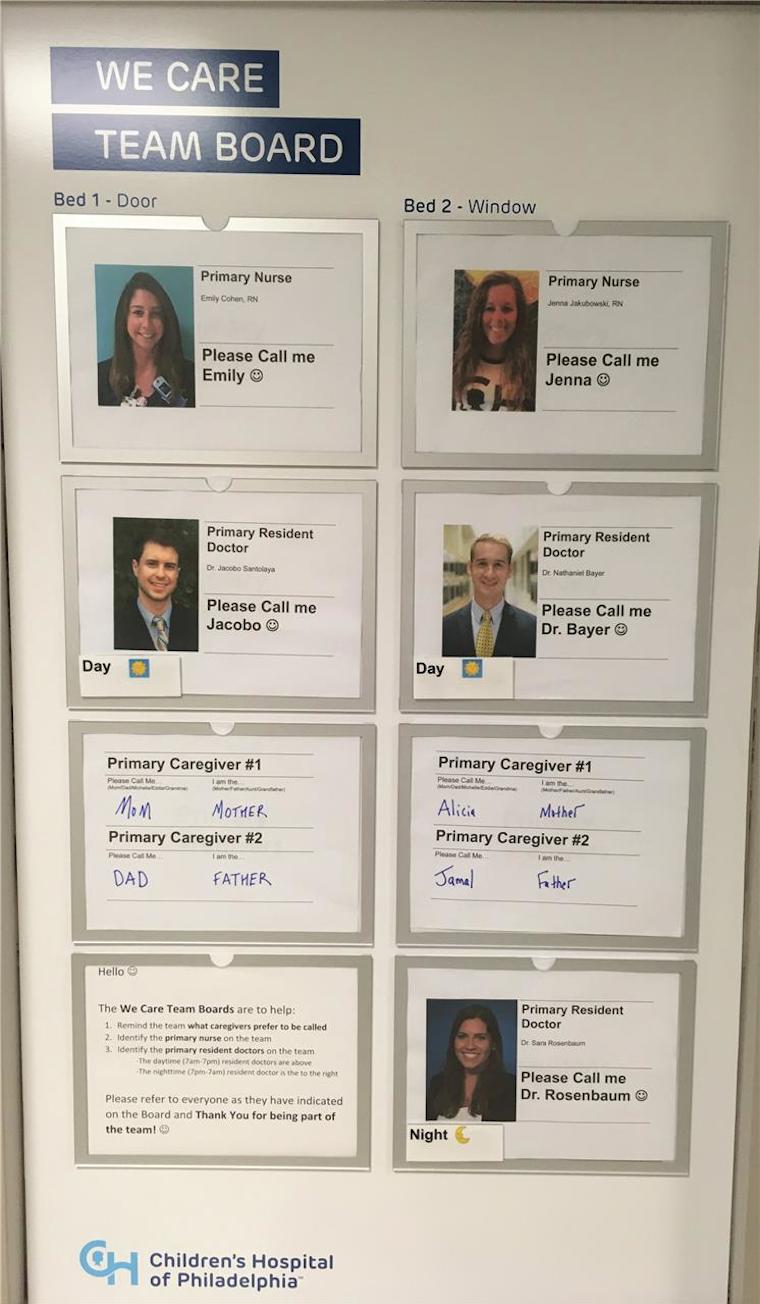
That finding led the team to install a board outside each patient’s room to note not only the caregiver’s name and relationship to the patient, but also the caregiver’s preferred name, as a way to encourage closer connections between caregivers and residents.
It is also a two-way street. Residents’ names and photos were posted outside the door, so caregivers could identify people on the patient’s care team and know their roles. Residents have reported that it is gratifying when parents know their names and can extend a more personal greeting.
“I got into medicine for the same reason everyone else does: to help people,” said Dr. Bayer. “If our time with patients is limited, then it becomes critical that we maximize that time and engage with patients immediately and on a personal level. A simple thing, such as using each other’s preferred name, can really make a difference.”
Said co-lead Dr. Santolaya: “One of the most exciting parts of this was seeing it implemented. After the boards went up, we started receiving great feedback that this was an important – but often overlooked – concept. This idea that calling someone by their name can mean so much. And it’s significant to both sides, the patient and families, but also to residents.”
The data collected showed an uptick in the quality of and satisfaction in resident/caregiver interactions. The team is considering spreading the intervention to other areas of the hospital. Dr. Bayer has graduated from residency and is now a pediatric hospitalist at the University of Rochester, Golisano Children’s Hospital. He is continuing to lead efforts to strengthen the provider-family relationship based on his experience co-leading this project.
The program is part of the ACGME Back to Bedside initiative, which empowers residents and fellows to develop transformative ideas and projects that foster meaning and joy in work through deeper engagements with patients. The initiative provides financial and administrative support to innovations that can be broadly disseminated and solutions that can be implemented at multiple institutions. More than 60 projects across two cycles have received initial funding through Back to Bedside.
Back to Bedside was created in response to the trend of patient care and academic learning occurring away from the patient bedside. External pressures, including administrative burdens, electronic health record requirements, production pressures, built-in inefficiencies, and other local influences are responsible for this shift in the delivery of medical education and patient care.
Back to Bedside hopes to support processes, initiatives, curricula, projects, or other activities designed and implemented by and for residents and fellows. By fostering activities that build a sense of meaning in work and reminding them of the reason they entered the profession in the first place, this initiative hopes to encourage all residents and fellows to look at how they can improve their learning environments.